COURSE DESCRIPTION:
The course begins with a unit of instruction on general anatomy and radiographic positioning terminology/nomenclature. The course then introduces the beginning radiography student to a study of the anatomical structures and basic functions that relate to the: radiographic examination of the chest for heart and lungs (thoracic viscera), the abdomen (digestive, biliary and urinary systems) and the upper extremities. Principles of radiographic positioning and procedures involved in the preparation, examination and evaluation of the aforementioned anatomical structures, are presented for student learning. Units of instruction also include mobile radiography, pediatric radiography, geriatric radiography and trauma radiography.
Prerequisite: Admission into the Radiography Program.

Unit 1 Examination Review
- read/review Chapter 3 of Merrill's
- read/review Mallett pgs. 4 and 5
- review homework assignment from workbook
- complete Chapter 44 of The Integrated Radiography Workbook (DeAngelis) and review the question explanations at the end
Know opposites: proximal - distal, inversion - eversion, pronation - supination, internal - external, recumbent - erect (upright), medial - lateral, vertical - horizontal, ventral - dorsal
A plane dividing the body in anterior and posterior sections is a coronal plane (equal anterior and posterior = midcoronal)
A plane dividing the body in superior and inferior portions = transverse (horizontal plane)
A plane dividing body into right and left sections is a sagittal plane (equal right and left = midsagittal plane (MSP) )
body habitus = classification of an individual's size/shape
asthenic - thin - stomach long and vertical, colon in pelvis, lungs long
hypersthenic - large/massive build - stomach - high and transverse, colon along periphery of abdomen, lungs broad and short
ventral decubitus - patient is prone
dorsal decubitus - patient is supine
anatomical position - patient standing with palms facing forward
proximal - towards point of attachment (i.e. the elbow is proximal, the wrist is distal)
distal - away from point of attachment (i.e. the ankle is distal, the knee is proximal)
extension - increase angle of joint
flexion - decreases angle of joint
tangential projections - central ray skims a body part
towards the midline of the body = medial
away from the midline of the body = lateral
projection = path of the x-ray beam from tube through the patient's body to the IR
abduction - moving arm away from central axis of body
adduction - moving arm towards central axis of body
RAO/LAO position = PA oblique projection
RPO/LPO position = AP oblique projection
decubitus projections require the x-ray beam to be horizontal, used to demonstrate air/fluid levels
Trendelenburg - head lower than the feet
lordotic = AP projection with superior chest tilted back towards bucky
Study Hard! Good Luck!!!

Unit - Anatomy and Positioning of the Respiratory System
Unit Learning Objectives - Anatomy and Positioning of the Thoracic Viscera
At the completion of this unit, the student will be able to:
1. List the structures constituting the airway through which oxygen will pass as it travels from the mouth/nose to the distal aspects of the lungs.
- Identify structures on anatomical drawings.
2. Name the structure serving as a common passageway for both food and air and be able to list the individual anatomical parts.
3. List the skeletal landmarks associated with certain organs of the respiratory system.
4. Identify which bronchus food particles are more likely to enter and list the reason why.
5. List the number of lobes in each lung and identify their correct names.
6. Identify which hemidiaphragm is higher and list the reason why.
7. Identify on drawings, the major anatomical portions of the lungs in both a frontal and lateral
position.
8. Identify the correct term describing the space in the thoracic cavity between the lungs and list the
various organs contained within this space.
9. Identify the correct term used to describe the double walled membrane enclosing each lung and its various parts.
10. List the functional unit of the lung.
11. Define “fissures” and be able to locate the oblique and horizontal fissures of the lung.
12. Understand the basic physiology of respiration.
13. Given a definition, identify the following terms: atelectasis
bronchiectasis
bronchitis
laryngitis
pneumonitis
bronchopneumonia
pleurisy
pleural effusion
empyema
hemothorax
pneumothorax
tracheotomy
lobectomy
pneumonectomy
thoracocentesis
14. Identify those parts of the bony thorax which are present in chest radiography.
15. List the number of ribs which should be present/demonstrated above the diaphragm on a well positioned P.A. chest radiograph.
16. List various reasons why chest radiographs should be taken with the patient in an upright position, whenever possible.
17. Describe/identify motion on a chest radiograph.
18. Explain why a 72 inch SID is desirable for chest radiography.
19. List the routine chest projections done at most institutions.
20. Understand the importance of full inspiration for chest radiography.
21. Understand the importance of inspiration/expiration films on a patient with a suspected
pneumothorax.
22. List the radiation protection measures which should be utilized in chest radiography.
23. Identify the CR location for a properly positioned PA/Lat. chest.
24. List various questions which should be asked of the patient before chest radiography.
25. Understand why a left vs. a right lateral projection is desirable.
26. List the primary side of interest for chest obliques.
27. List the amount of pt. obliquity for properly positioned chest obliques.
28. Describe/understand the importance of the following special chest positions: decubitus and lordotic
29. Successfully pass a laboratory competency examination for chest radiography.
30. Understand all lectured and required reading materials, pertinent to this unit.
Respiratory System Anatomy
Great website to review respiratory system anatomy -
http://www.getbodysmart.com/ap/respiratorysystem/menu/menu.html
Path of air as it travels proximal to distal in the respiratory tract:
Nasal cavities>pharynx (oro-, naso-, laryngo-)>larynx>trachea>primary (main) bronchi>lobar bronchi>segmental bronchi>bronchioles>alveoli
The alveoli are the functional units of the lungs where the physiology of respiration actually occurs.
Right lung has three lobes, whereas the left only has two.
The right lung has two fissues (oblique and horizontal) separating it into the right superior lobe, right middle lobe and right inferior lobe.
The left lung has only the oblique fissure separating it into the left superior lobe and left inferior lobe.
Parietal pleura - lines the chest cavity
Visceral pleura - covers the lungs directly
pleural cavity - between parietal and visceral pleura
apex of lung = superior portion
base of lung = inferior portion
hilum = medial portion
costophrenic angle (CPA) = outer lower corners of lungs where inner surface of lower chest wall and diaphragm are in contact
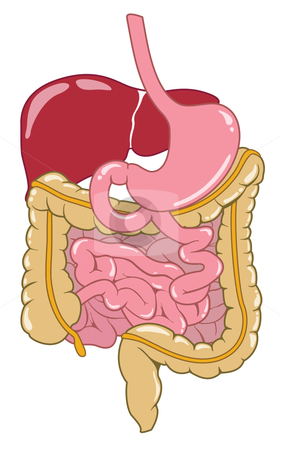
Unit - Anatomy and Positioning of the Abdomen
Unit Objectives - Anatomy and Positioning of the Abdomen
At the completion of this unit, the student will be able to:
1. Identify on drawings and radiographs, the anatomy of the principle organs and structures of the digestive system, liver and biliary systems, pancreas, spleen, urinary system and adrenal glands.
2. Localize all organs as identified in objective #1 to one of four quadrants of the abdomen.
3. Identify and describe the position of the important bony landmarks used in positioning for the abdomen.
4. Describe the relationship of the bony landmarks to other skeletal structures.
5. List and describe the muscles of the abdomen.
6. List those structures which should be visible (in reference to soft tissue differentiation) on a correctly exposed abdominal radiograph.
7. Identify two bony landmarks which should be used to position a supine and prone abdomen.
8. Divide the abdomen into nine regions and be able to name each region.
9. Simulate an abdominal radiographic examination.
10. List various types of pathology which would indicate a need for an obstruction series/ three-way abdomen/acute abdomen series/free-air series.
11. Identify which lateral decubitus should be taken if there is a question of free air in the abdominal cavity.
12. Given diagrams and/or radiographs of various body habiti, identify the type according to Mill’s classifications.
13. Briefly explain the term KUB and Flat-plate of the abdomen.
14. List the IR size and direction of each IR for the following examinations of the abdomen: supine and free air series.
15. Identify the structures on each projection of the examinations listed above.
16. List various steps involved in positioning the body for each projection of the above listed abdominal examinations.
17. List various protective measures employed to reduce radiation exposure to the patient during these examinations.
18. Record various questions that a patient must be asked in order to obtain a thorough history.
19. List the reasons why a patient should void prior to a radiographic examination of the abdomen.
20. Record the desired scale of contrast for abdominal examinations.
21. List the structures which are demonstrated when an abdomen in the lateral position is taken.
Digestive System Anatomy
Great websites/videos to review digestive system anatomy
http://www.acm.uiuc.edu/sigbio/project/digestive/index.html
http://www.youtube.com/watch?v=MVt9dW0c9FM
http://www.youtube.com/watch?v=Z7xKYNz9AS0&feature=related
Essential to success with pediatric patients:
-Understanding that children are not small adults
Provide distractions to reduce anxiety:
Parent Participation:
Depends on:
Preteens and adolescents = able to understand
- Often worried about recovery
- Need clear explanation and questions answered
- Sensitive issues arise due to possibility of pregnancy, since menstruation onset varies
Will physical limitations influence the way the examination is performed
Many inpatients are on a 24-hour urine and stool collection
Special Concerns including pediatric patients with the following:
Protection of child from injury:
- Perform routine safety inspections

Unit Objectives - Anatomy and Positioning of the Fingers, Hand and Wrist
At the completion of this unit, the student will be able to:
- Identify on both drawings and radiographs all of the anatomical structures of the fingers, hand and wrist.
- List all of the names of each carpal bone.
- Identify the joints of the fingers, hand and wrist and list the classification of each joint.
- Identify and describe the basic projections and central ray locations for the thumb, finger, hand and wrist.
- Describe the condition “carpe bossu” and identify the projection which will best demonstrate this condition.
- Describe the specialized projection taken for the scaphoid (navicular).
- List the conversion factors for radiographing casted extremities.
- Position on a fellow student all of the basic projections for thumb, fingers, hand and wrist.
- Describe various means of reducing/eliminating motion on radiographs of the hand/wrist.
- List reasons why close collimation is important in radiographing the extremities.
- Understand the importance of using a small focal spot when radiographing the fingers, hand or wrist.
- Identify the reason why it is preferable to radiograph the thumb utilizing an AP versus a PA projection.
- Describe the appearance of the anatomical structures of the fingers when a PA oblique hand is radiographed using a sponge finger support versus placing the fingers directly on the cassette.
- Describe the difference in the radiographic appearance of the PA wrist when it is radiographed using ulnar deviation (flexion).
- Describe the Gaynor Hart Method and identify the anatomical structures which are best seen.
- Identify the radiographic position which is the customary projection for the demonstration of foreign bodies in the hand.
- Describe the Norgaard Method and Stecher Methods and identify the pathology/condition which is best seen using this projection.
- Identify the customary projection of the hand used to demonstrate anterior or posterior displacement of the metacarpals.
- Identify various reasons why the carpal bridge projection may be taken.
Great Websites for learning anatomy of the Fingers, Hand and Wrist:
http://www.assh.org/Public/HandAnatomy/Pages/default.aspx
http://chionline.com/anatomy/anat4.html
http://www.youtube.com/watch?v=Z6jUzWUGcOs - Great video for finger, hand and wrist anatomy!
Mobile Radiography
Mobile radiography uses transportable x-ray equipment to bring imaging services to the patient
- Commonly performed in patient rooms, emergency departments, intensive care units, surgery and recovery rooms, and nursery and neonatal units
- Mobile x-ray was first used in the military -Units were carried to field sites
- Some machines have preset anatomic programs (APRs) similar to stationary units
- Automatic exposure control (AEC) is also available for mobile units
- Mobile units with direct digital capability
- Flat panel detector connected by a cord or communicates through wireless technology
Inform all persons in area that exposure is going to be made
Orthopedic beds, fracture frames, tubes, wiring, etc., produce artifacts
IR cover makes positioning easier because cover does not stick to skin